Difficult Airway Course Curriculum
CME course when and where you want it!
The up to 7 hour AOD airway workshop is designed to present the clinician with the same materials covered in a two day conference. Additionally, the course is given locally and at a choice of date in order to eliminate travel costs and minimize lost work time.
Airway Course Objectives
After attending this workshop the learner will be able to:
- develop an appropriate airway management plan based on the findings of a focused medical history and airway physical exam, and apply these plans to patient care;
- apply principles of advanced airway evaluation to the synthesis of an appropriate airway plan;
- design and administer a conscious sedation plan
- apply a plan for failed conscious sedation
- assess their performance of airway rescue and routine tracheal intubation with the incorporation of modern optical/video devices;
- assess their performance of airway rescue and routine airway management with the incorporation of modern supraglottic airways;
- apply patient preparation techniques in the performance of awake tracheal intubation;
- apply techniques of minimally invasive airway rescue;
- evaluate the potential for failed tracheal extubation and develop a plan for emergency reintubation.
ASC, OMF and Emergency Medicine Courses:
The above objectives and curriculum is customized to specialty. Courses for ASC, OMF and EM specialties include lectures and hands on training in:
- Prevention of hypoxia, hypoventilation and apnea
- Monitoring for hypoxia, hypoventilation and apnea
- Basic airway maintenance and rescue
- Advanced airway management including RSI
- The course is divided into didactic and hands-on/simulation sessions
Airway Workshop Didactic Curriculum (the curriculum is flexible and designed for the learners present)
The lectures are multimedia in nature. Nearly all techniques are demonstrated in actual patients. Based on the needs of your group, the curriculum for your event may vary from that of below.
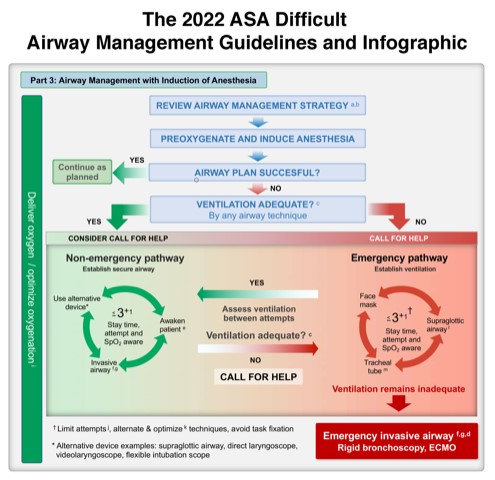
- Decision Making in Airway Management and Advanced Airway Evaluation
This lecture describes the process of integrating available patient information along with the clinician's experience with airway management techniques in order to design a rational airway plan for all patients requiring airway management. Topics include 1) the need for airway control, 2) evaluation for difficult laryngoscopy, 3) evaluation for supralaryngeal airway ventilation, 4) aspiration risk, and 5) evaluation of
judgment error
risk. Advanced airway evaluation. - Conscious sedation and failed conscious sedation, including monitoring (O2sat, ETCO2, Impedance monitors) and basic airway maneuvers (head tilt, chin lift, oral aw, nasal aw, mask vent, tracheal intubation)
The decision making concepts of the first lecture are applied to the patient with undergoing conscious sedation.
- Break
- The Pediatric Airway / Obstetric airway
The difference between adult and pediatric anatomy is reviewed. The rationale for eliminating certain "adult" techniques from the pediatric airway armamentarium, and unique pediatric techniques are discussed.
- Aids to Direct Laryngoscopy (e.g., bougie, positioning and laryngeal manipulation)
Techniques and devices which can be employed when direct laryngoscopy fails are reviewed
- Awake Intubation
When it has been determined that the patient requires a technique of awake intubation, several distinct factors must be addressed, and a plan formulated. These factors include: 1) explanation to the patient, 2) drying of airway secretions, 3) nasal vasodilatation, 4) planned airway analgesia, 5) sedation, and 6) time management. The importance of weighing these 6 facets equally is emphasized.
- Flexible intubation scope (e.g., FOB) intubation
Successful use of the flexible intubation scope depends on an understanding of the construction of this highly engineered device, as well as the pitfalls of its use. This lecture explores the mechanics of the fiberscope and how it is best manipulated for maximum control. Patient pathology and the obstacles which are encountered are reviewed.
- Other Indirect Vision Devices (Video Stylet, Video Laryngoscopes, Channel Scopes, etc.)
Rigid, malleable, and distal camera devices have recently been added to the armamentarium of the airway manager. The role of these devices is reviewed, including specific situations where each may have an appropriate application. Every new medical technology has the potential to introduce new complications. This is very true of the video laryngoscopes, and is highlighted.
- Break
- Supraglottic Airways
The ASA task force on the difficult airway has recognized that SGAs must become a mainstay of airway management. In 2003, their status was elevated from the role of
emergency airway rescue
toroutine devices
. In 2013, it was recognized that SGAs other than the classic LMA also play a role. The rationale for the new prominence of SGAs, as well as the tremendous variety of these devices, will be discussed in the context of difficult airway management, as well as how they can improve routine practice. - Minimally Invasive Airway Management
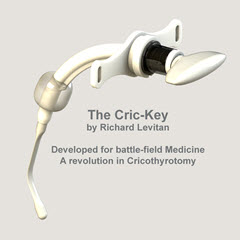
When a patient's airway fails and cannot be managed by routine means, the ASA recommends that invasive measures are instituted. In fact, the ASA Closed Claims database recognizes that a major cause of patient morbidity is the delayed institution of these techniques. This does not mean that the anesthesiologist must be able to perform a surgical airway! Minimally invasive techniques of Transtracheal Jet Ventilation and Percutaneous Cricothyroidotomy are relatively simple techniques.
- The Vortex Approach
A new concept in managing the failed airway, the Vortex Approach was introduced as a cognitive aid when working with multiple team members in an airway code when it is near impossible to follow published algorithms. The Vortex Approach is also incorporated into the AOD simulation course.
- Extubation of the Difficult Airway
The Closed Claims database has recognized that, subsequent to the publication of the ASA algorithm, morbidity occurring during intubation has fallen. Unfortunately, there has been little change in morbidity occurring during tracheal extubation. Recent data has shown that reintubation failure can occur in 72% of patients. Most airway courses fail to address this issue. This course will discuss a rational plan for pre-extubation assessment of airway patency and techniques aimed at facilitating reintubation
Hands-on Airway Workshop
Enough materials are provided to allow clinicians unhurried exposure to all techniques within a two hour period. Though a work/check off sheet may be provided with the syllabus, there is no regulation of the time spent at each station. It is the AOD philosophy that not all devices must be mastered. Rather, the clinician should be familiar with one or more of each of the following categories: indirect-optic, SGA and percutaneous technique. The ratio of (scheduled) attendees to stations is at most 6:1.
The following stations are available at all AOD workshops:
- Flexible intubation scope
- Rigid or malleable fiberoptic*
- Laryngeal Mask Airway varieties
- Intubating SGAs
- King LT
- iGel
- Aura
- AirQ (Cook-gas)
- Retrograde wire intubation
- Percutaneous cricothyrotomy
- Glidescope
- McGrath
- Airtraq
- Pentax Airway Scope
- Others
*(e.g, one or more of: Video Macintosh, Bullard, Shikani, Glidescope, Airtraq)
When elected, an airway simulator will be available (AirMan or SimMan)
Teams of one to three clinicians will complete successful
and failed
airway scenarios. Scoring and feedback emphasis will be directed towards decision-making and team management, not device technique, which is better learned on partial task trainers. Completion of the simulation station is not mandatory for AOD course credit.
When elected, swine trachea lab will be available
Each attendee will work on a pig trachea fixed to a surface and (when available) covered by pig skin. This model will be used for the practice of trans-cricothyroid needles placement and placement of a Melker critothyrodotomy.